EHS Secretary General, Professor Eleftherios Tsiridis

The 3rd wave has hit Europe and according to the *ECDC Europa data, hospital and/or ICU occupancy and/or new admissions due to COVID-19 have increased compared with the previous week in 27 countries (Austria, Belgium, Bulgaria, Croatia, Cyprus, Czechia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, the Netherlands, Norway, Poland, Romania, Slovakia, Slovenia, Spain and Sweden. NB Daily data availability varies.)
However, the weather will be improving from now on and of course the vaccine is rolling out steadily across Europe. Things can only get better. Yesterday the University of Oxford’s research team released news of a finger-prick antibody test – the culminative work of scientists from UK, Taiwan, India, Thailand and France.
Please enjoy the Diary of an Orthopaedic Surgeon facing COVID-19 in Ireland, from our EHS Nat Rep for Ireland, Prof Derek Bennett. Please contact the EHS Secretarial Office via our Membership Secretary (samstokesehs@gmail.com) with reports on the COVID-19 developments in your area which you would like to share directly with our fellow hip surgeon members. Thank you.
The Covid Pandemic: reflections from an Irish hip surgeon, by Derek Bennett

One year on and it’s hard to believe how much the world has changed for the people of this small island. Ireland sees itself as a natural bridge between the continents of Europe and America and the desire to travel the world is embedded deeply in the Irish soul. How ironic that so many of the freedoms we took for granted have now been curtailed by the global travel of a novel microorganism.
By St Patrick’s Day last year, the extent of the gathering storm was becoming apparent although knowledge of the full nature of our microbial adversary was limited. It was clear that preparations would have to be made on many fronts. In particular, there was a very real concern that our health services might become overwhelmed. We saw the effects of the virus in Wuhan and then closer to home in Italy. We clearly lacked hospital capacity, Intensive Care beds and ventilators, personal protective equipment. We feared that our carers themselves would fall victim to the virus.
With the evident support of the nation, the Government set about first restricting the virus’ ability to spread through the population. Entire industries were shut down: tourism, construction and education. Many other sectors were severely restricted and non-essential travel within the country was prohibited. That essential component of community life, the Irish Pub, was forced to close. Restrictive measures have periodically relaxed and tightened according to the ebb and flow of the virus numbers.
At the same time, steps were taken to strengthen the health service capacity to deal with the pandemic. All non-urgent surgical activity was cancelled. All private hospitals were taken over entirely by the state for a period of 3 months. The dormant surgical capacity in public hospitals was used to increase capacity for treating Covid patients and surgical territory including operating theatres, anaesthetic rooms and post anaesthesia care recovery areas were repurposed to be used as temporary intensive care units. The country joined the global scramble for Personal Protective Equipment and our airlines carried facemasks instead of tourists. Final year medical students were given 3 days notice that their exams were to be brought forward by over a month and a worldwide campaign to recruit Irish healthcare workers who were overseas attracted more than 70,000 applicants within weeks. A darker aspect of the same policy was that retirement from the police force was prohibited and all police recruits were subject to accelerated training and qualification so that they could be rapidly deployed.
The summer brought a period of calm in the storm. Numbers of infections dropped. We learned that our most vulnerable people were the residents of elderly care facilities and we learned that we could only protect them by isolating them. Tourism and construction were allowed to resume although subject to strict controls and education became a remote learning experience with few in person learning experiences. Gradually, elective surgery resumed in the public hospitals and state control of the private hospitals was relinquished. The private hospitals generally became “non-Covid” hospitals, primarily for elective surgery with strict isolation measures for 2 weeks prior to planned admission as well as PCR testing prior to admission for all patients and regularly during their hospital stay. The public hospitals remained as mixed Covid and non-Covid hospitals. Attempts to segregate Covid and non-Covid patients have had variable success.
The virus waxed and waned during the autumn with a second wave reaching a peak in October. A further easing of restrictions to allow some Christmas celebration coincided with the arrival of the B117 variant. Free travel to and from the United Kingdom and the many close family ties with our British neighbours meant that this rapidly became the dominant variant in Ireland and a further severe lockdown was necessary in early January. Again, elective surgery in public hospitals was the first casualty but on this occasion the “non-Covid” private hospitals were able to continue their work almost without interruption. The numbers of Covid cases have dropped to a steady plateau and although this is higher than the number of cases last year it is at a level where our health service is not currently threatened with being overwhelmed. Gradually, elective surgery is resuming over the last few weeks and we are optimistic that this will continue.
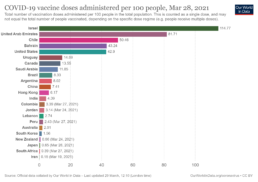
Roll out of the vaccines began quite hesitantly at the end of December. Initially, healthcare workers and residents of elderly care homes were prioritised and at this stage the priority is elderly citizens in our community and in particular in our hospitals. The vaccine delivery has been slower than in our neighbouring countries: the United Kingdom to the east and the United States to our west and it is clear that our decision to order vaccines from the manufacturers was delayed because of uncertainties about safety and efficacy. Fear of making a wrong decision permitted procrastination about making any decision. For all its limitations and failings, the vaccination programme remains our best and only hope of returning to a normal life.
We have all had to learn quickly over the last 12 months and I hope that with that practical knowledge will come wisdom. I have been struck by the fortitude, compassion and resilience of healthcare workers. I am proud and at the same time humbled to have been able to make a contribution to our response to the pandemic.