EHS Secretary General, Professor Eleftherios Tsiridis

Travel is finally opening up between many countries and the World Health Organization reported that global Covid-19 cases fell by 14% last week (4.1m global Covid-19 cases were reported in the week ending May 23) and deaths were down 2%. Other good news is that the Moderna vaccine is considered safe and effective in adolescents.
However, our thoughts and prayers remain with the people of India, who have been so terribly hard hit by COVID-19 (cases surpass 27m) and are now facing the added abomination of the mucormycosis infection (cases surpass 10,000k), believed to be linked with the steroids used to treat COVID-19 and hitting up to 18 days after recovery from COVID-19.
Meanwhile, and in striking contrast, a good news report from our EHS International Member in New Zealand, Dr Nemara Sandiford, who writes a Diary of an Orthopaedic Surgeon during the pandemic this month. Thank you very much to him.
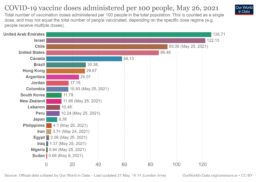
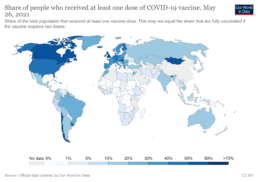
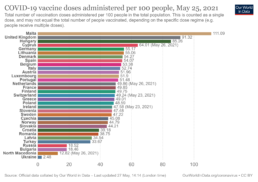
Below is the update of the vaccination progress in our EHS member countries across the world, taken from Oxford University’s Our World in Data. Meanwhile, please do contact the EHS Secretarial Office via our Membership Secretary (samstokesehs@gmail.com) with reports on the COVID-19 developments in your area which you would like to share directly with our fellow hip surgeon members. Thank you.
The impact of COVID-19 on the delivery of Orthopaedic Surgery: a view from New Zealand, by Mr Nemandra Sandiford

It is a pleasure and a privilege to address the membership of the EHS. My practice is based in a regional teaching hospital in the South Island of New Zealand where I moved to from London in 2019. I will share our experience of attempting to deliver high quality orthopaedic care during the pandemic.
New Zealand (NZ) consists of 2 main landmasses (the North and South Islands) and over 700 smaller islands. The main international airports are located in both islands: Auckland and Wellington in the North Island and Queenstown and Christchurch in the South Island. The greatest population density occurs on the North Island in Auckland.
New Zealand observed solemnly the spread and devastating impact of the COVID-19 pandemic in early 2020. The exponential speed of transmission as well as the benefits of social distancing and isolation became evident early in the evolution of the pandemic. In NZ, our leaders acted early and decisively to manage traffic at the borders and a national lockdown was enforced between March and May 2020. The country’s population was kept informed with daily updates from political leaders as well as the Chief Medical Officer. The National Emergency Mobile Alert was used to remind the population when lockdown periods started, changed and their levels. Instructions were clear. In total 2669 infections were recorded with 26 deaths (a mortality rate of 0.01%).
To date, 3.9% of the population (total population: 4,857,451) have been fully vaccinated and 7.5% have received the 1st of 2 vaccines. The people of New Zealand have co-operated with the recommendations and advice of their decisive leadership.
I have undertaken fellowship training in arthroplasty in Vancouver, Exeter, London, Nijmegen and work in a department with a combined medical experience of almost 100 years, yet nothing could prepare us for this! Some of the main issues of this century and the last have resulted from violent conflicts. In this setting orthopaedic surgeons have comprised the frontline of care providers. In the setting of a viral pandemic however, we quickly realised that our main role was to provide support to our colleagues in general medicine, emergency medicine and general practice. We split our teams in order to minimise our own exposure (and keep patients safe) and learnt to manage patients remotely. We experienced triaging in an emergency situation and witnessed the effectiveness of conservative management of many common trauma presentations. This is counterinitiative to many younger surgeons who have ‘grown up’ in the era of operative fixation of the majority of commonly presenting fractures. Sir John Charnley’s ‘The Closed Treatment of Common Fractures’ had possibly never reached the heights of popularity within our department as it did during this period!
We provided emergency surgery where required but arguably the most important aspect of care during the lockdown period was to stay in touch with patients via virtual clinics, keep them informed that they were important to us and were being cared for. I felt this was very important especially at a time when people were isolated in their homes.
During lockdown our registrars performed more procedures than many of their peers nationally. We were always aware of our duty to train our junior colleagues.
It is only too easy, and understandable, to focus on the negative aspects of the COVID-19 pandemic, as there are many. There have been valuable positives which can also be taken out of this period however. These are also worthy of mention.
We have learnt the value of modern technology in helping us with our daily work. We have learnt to harness technology in order to be productive and provide care for our patients in exceptional circumstances and in continuing to learn and grow in our own practices. Many of us, myself included, have seen, first hand, the vital importance of teamwork and collegiality, whether this was simply helping an overworked colleague or sharing vital data internationally in order to save lives. The concept of who is an ‘essential worker’ has been at the forefront of many debates. This issue is important and humbling as it reminds us that we all have value, and should value others. The wonderful persons who work hard to keep our hospitals, streets and cities clean and disease free deserve the same care and compassion as the Professor of Orthopaedic Surgery.
Above all, we have learnt the absolute critical importance of the human connection that is as important as our careers in orthopaedic surgery. Many of us have missed the company and ability to interact with friends and colleagues.
I hope it is not overly optimistic to say that there does seem to be some light at the end of the long dark tunnel COVID-19 has created in our world and our lives. I look forward to seeing many of you at conferences, meetings, courses and all the wonderful activities which fulfil and enrich our professional lives.
NA Sandiford MSc FFSEM FRCS (Tr/Orth)
Consultant Orthopaedic Surgeon
Southland Teaching Hospital
Invercargill, NZ